Abstract
Background
Ploidy is a highly significant prognostic factor in childhood acute lymphoblastic leukemia (ALL). Children with hypodiploid ALL continue to have inferior outcomes despite current intensive chemotherapy treatment. Hypodiploid ALL is divided into two groups based on genetic alterations. Near-haploid ALL with 24-31 chromosomes harbors alterations targeting receptor tyrosine kinase signaling, RAS signaling, and the lymphoid transcription factor gene IKZF3 and low-hypodiploid ALL with 32-39 chromosomes is characterized by alterations in TP53 that are commonly present in non-tumor cells, IKZF2 and RB1 . There is little information about children with hypodiploid ALL in Asia including Japan, although ethnic differences seem to exist. The aim of this study was to clarify the clinical characteristics and outcome of pediatric hypodiploid ALL in Japanese patients.
Methods
Patients with fewer than 46 chromosomes were defined as hypodiploid ALL in this study. All reports of chromosomal analysis were re-reviewed by two independent investigators and 117 cases of hypodiploid ALL were identified out of 4261 patients who were registered in clinical trials between 1997 and 2012. A total of 64 patients were excluded due to the lack of follow-up data (n = 39), only a single cell exhibiting a chromosome number less than 46 in G-banding experiments (n = 18), incorrect diagnosis (n = 4), or congenital chromosomal aberrations such as Down syndrome (n = 1) and Robertson translocations (n = 2). Seventeen patients whose karyotypes at remission were not evaluable were also excluded.
Results
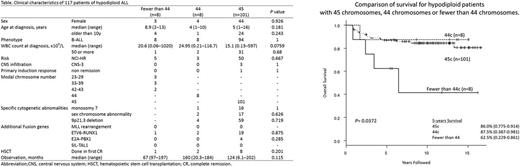
In total 66 male (56.4%) and 51 female (43.6%) patients' data was evaluated with a median age of 6 years (range 1 to 15 years). There were 101, 8, 2, and 3 patients with chromosome numbers of 45, 44, 43, and 36, respectively. One patient exhibited each with 27, 28, and 29 chromosomes. No patients had a modal chromosome number of 30-35 or 37-42. Among the 117, 110 (94%) had B-precursor ALL and 105 (90%) had CD10 positivity. All T-ALL patients (n = 7) had 45 chromosomes. Out of 117 patients, 22 were TEL-AML1 fusion positive of which 19 had 45 chromosomes, 2 had 44 chromosomes, and 1 had 43 chromosomes. There were no patients with central nervous system (CNS) infiltration at the time of diagnosis. All but one patient who was diagnosed with T-ALL achieved a complete remission (CR) with a CR rate of 98.3%. Overall survival at 5 years varied significantly at 86.0%, 87.5%, and 62.5% in patients with 45, 44, and fewer than 44 chromosomes, respectively (P=0.037). There were no patients with CNS relapse in both the 44 and fewer than 44 chromosomes groups. Five patients out of 8 with fewer than 44 chromosomes had bone marrow relapse, even though 1 patient had undergone hematopoietic stem cell transplantation (HSCT) during his first CR. Four patients underwent HSCT after relapse, but only 1 was cured. In the 44 chromosome group, 2 of 8 patients underwent HSCT during their first CR and did not show relapse. However, one of them developed secondary renal cell carcinoma 10 years after treatment. One patient with 44 chromosomes underwent HSCT after relapse and failed to be salvaged. We also analyzed some variables that influenced event-free and overall survival in the 45 chromosome group: monosomy 7, sex chromosome abnormality, and 9p21.3 deletion. We were not able to identify any significant prognostic factor among patients with 45 chromosomes.
Conclusions
Although the number of patients was small, patients with 44 chromosomes without HSCT showed better prognosis than those reported previously. However, the outcome of Japanese patients with fewer than 44 chromosomes was as poor as previously reported in other countries. The effect of HSCT in patients with hypodiploid ALL needs to be the subject of future studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal